Causes of hearing loss

There are many causes of hearing loss and a number of ways of explaining or classifying them. This article doesn’t include much about causes of hearing loss present at birth (congenital); it mostly covers hearing loss acquired from childhood onwards.
A straightforward way of categorising causes of hearing loss is based on the type of hearing loss and how it relates to which part of auditory or hearing system has become damaged or is in some way abnormal. Often, hearing loss is accompanied by tinnitus (noises in the head or ears) and sometimes by a balance problem.
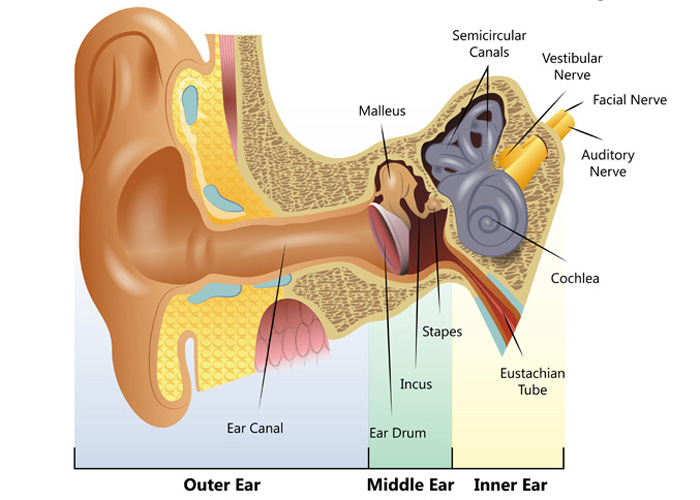
So, this article lists and briefly explains all the main causes of hearing loss affecting one or more of these four parts of the auditory system:
-
Outer ear
The outer ear which includes the external ear on each side of the head, sometimes called the pinna or auricle, the ear canal and the eardrum.
-
Middle ear
The middle ear which also includes the eardrum and the middle ear bones (called the ossicles or ossicular chain) within the middle ear cavity.
-
Inner ear
The inner ear which has two main sections, the cochlea for hearing and the vestibular system for balance.
-
Auditory cortex
The central auditory system which has highly complex nerve pathways connecting the cochlea (inner ear) to the hearing centres of the brain (auditory cortex).
Diagram of the human ear
Types of hearing loss
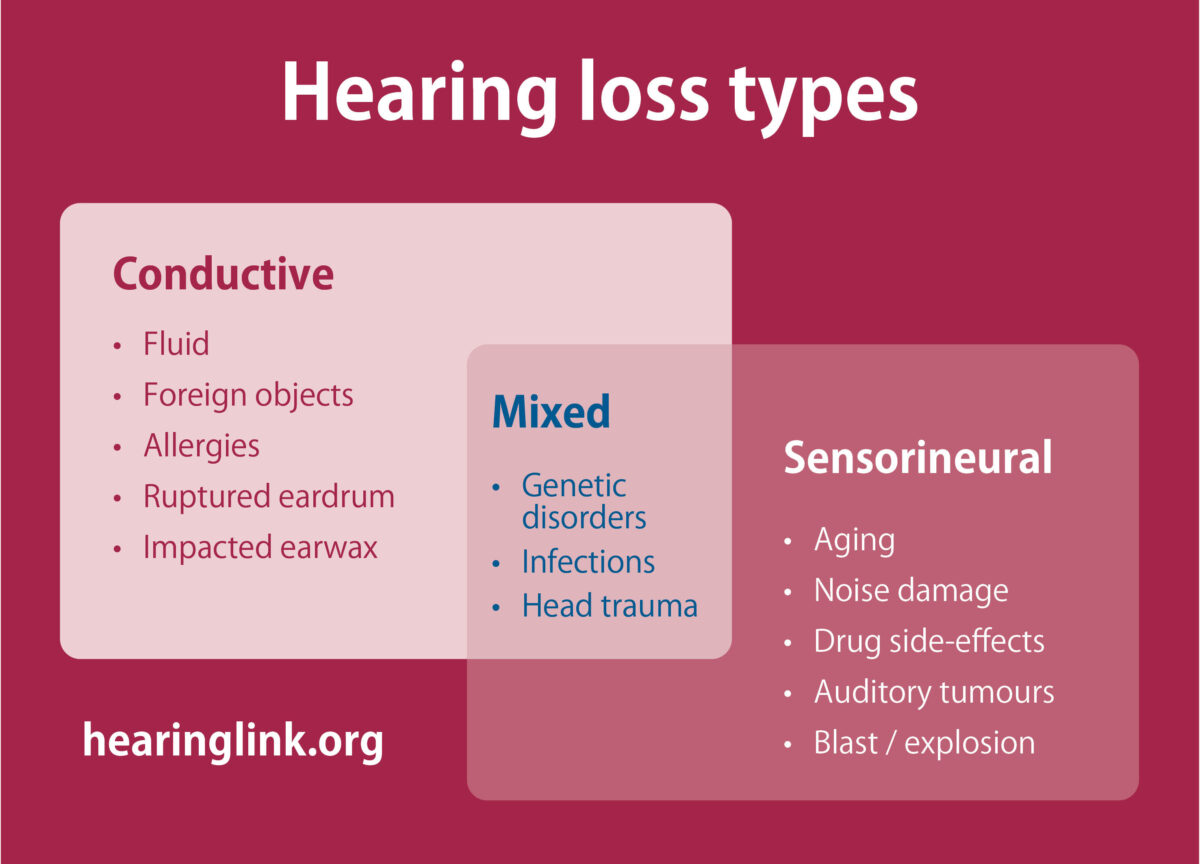
Conductive hearing loss
Conditions affecting the outer and/or middle ear cause conductive hearing loss which is often treatable and may, therefore, be temporary.
Sensorineural hearing loss
Disorders of the inner ear or central auditory system cause sensorineural hearing loss which is usually not medically or surgically treatable and is, therefore, generally permanent.
Mixed hearing loss
When there is both a conductive and sensorineural loss, this is called a mixed hearing loss.
The onset of a hearing loss can be sudden (within a few days), rapid (within a few months) or slowly progressive (over years rather than months). Sudden hearing loss is classified as a medical emergency and should always have urgent, hospital treatment.
Causes of conductive hearing loss (outer and/or middle ear)
Causes of conductive hearing loss (outer and/or middle ear) | |
Trauma & inflammation | The external ear (pinna or auricle) can be damaged by trauma or inflammation or there can be a congenital abnormality, i.e. present at birth.
Noticeable hearing loss will only arise if the entrance to the ear canal is obstructed or closed up preventing sound entry. |
Wax | The ear canal conveys sound to the eardrum. So, any blockage in the ear canal prevents sound transmission.
Excessive wax is the most common cause of hearing loss. |
Otitis externa | Any swelling in the ear canal due to allergy, skin infection or inflammation (called otitis externa) can affect hearing.
The eardrum is a delicate membrane which divides the outer from the middle ear, so it’s really part of both. The eardrum, as part of the outer ear, can easily be affected by infection or inflammation of the ear canal (otitis externa). |
Foreign body | Naturally, foreign bodies in the ear canal can block the passage of sound. |
Osteoma | Although not usually sufficiently large to cause hearing loss, bony growths can develop in the ear called osteoma.
If one or more of these grow to sufficient size, surgical intervention may be necessary to avoid hearing loss and other complications. |
Perforated eardrum | The eardrum is also vulnerable to perforation and subsequent infection if anything is pushed too far into the ear canal; hence the reason for all the warnings about using cotton buds in the ear canal!
Perforations of the eardrum are usually due to middle ear inflammation/infection (otitis media) usually resulting in a discharge from the middle ear into the ear canal as well as hearing loss. A blow to the side of the head, especially against the pinna, can cause the eardrum to rupture. |
Otitis media | A healthy middle ear cavity is filled with air and is ventilated by a narrow tube (the Eustachian tube) between the middle ear and the back of the nose.
So, nasal congestion, commonly with a head cold or from a variety of bacterial or viral infections, can prevent the Eustachian tube from supplying air to the middle ear and draining any fluid which encourages middle ear inflammation and infection (otitis media). This is a particular problem in young children but also affects adults. Otitis media affects the health and function of the eardrum and the ossicular chain; it is the most common cause of middle ear hearing loss. |
Cholesteatoma | Although affecting the eardrum as well, a potentially dangerous condition, which can impact all structures in the middle ear and beyond, is cholesteatoma.
It’s a benign growth which starts within a retracted section of the eardrum resulting from a sustained, abnormal middle ear pressure. It gradually enlarges, not only resulting in hearing loss but, if left untreated surgically, it can be life-threatening from complications such as mastoiditis and meningitis. |
Barotrauma | Any abnormal pressure in the middle ear cavity, due to inadequate ventilation and drainage of the middle ear cavity, can put the eardrum under such stress that it perforates.
Significant atmospheric pressure changes, such as when flying or diving, can cause pain and hearing loss sometimes resulting in eardrum rupture (called barotrauma). Flying or diving with a head cold increases the likelihood of barotrauma and can result in complications, even permanent hearing loss. |
Trauma | The chain of three tiny bones in the middle ear (ossicles or ossicular chain) transmit sound vibrations from the outer ear to the cochlea in the inner ear.
These tiny bones can suffer dislocation from head trauma such as in a road traffic accident or in contact sports such as boxing or rugby. |
Otosclerosis | Apart from the effects of middle ear inflammation and infection, the most common condition affecting the ossicular chain in adults is otosclerosis.
This is a hereditary condition but, because it doesn’t appear in every generation of an affected family, the genetic connection is often not obvious. The hearing loss becomes noticeable usually before the middle years of adulthood but is highly variable in onset. Fortunately, otosclerosis can be successfully treated surgically but, for those who do not wish to have surgery or where surgery is only partially successful, hearing aids are usually very effective. |
Causes of sensorineural hearing loss (inner ear to the brain)
As stated above, the inner ear has two sections, one for hearing (cochlea) and the other for balance (vestibular system). For this article, we are mostly concerned with hearing loss due to disorders in the cochlea but some conditions affecting hearing also affect balance.
It’s also the case that tinnitus can accompany almost all causes of hearing loss, especially those arising in the cochlea and/or centrally.
Causes of sensorineural hearing loss (inner ear to the brain) | |
Ageing (presbyacusis) | The effects of ageing are numerous. Age-related hearing loss is called presbyacusis and affects the majority of those over 60 years of age and certainly those over 70 years. It’s the most common cause of hearing loss.
All parts of the auditory system are affected by ‘wear and tear’ but particularly the cochlea and its associated nerve pathways to the brain. Typically, at least in the earlier stages, it affects hearing sensitivity to higher-pitched sounds which can have a marked effect on understanding speech especially in difficult listening conditions such as in background noise. Tinnitus is also frequently experienced. |
Noise exposure | Exposure to excessive noise is generally considered to be the second most common cause of hearing loss. The delicate sensory cells in the cochlea (called hair cells) can be damaged by loud noise. The higher the noise level or the longer the duration of exposure, the greater is the likelihood of permanent hearing loss often with tinnitus.
It’s no longer the case that noise-induced hearing loss (often abbreviated to NIHL) is mainly related to a noisy occupation or loud music at concerts. Increasingly, irreversible noise damage is from listening to loud music using earbuds or earphones with smartphones or other personal devices. NIHL is now affecting an increasingly younger age group. |
Cardiovascular disease | Cardiovascular disease is a significant component in age-related hearing loss. However, it can affect a person of any age when the blood supply to the inner ear or hearing centres in the brain is significantly reduced or stops altogether.
The cochlea in the inner ear is highly sensitive to a reduction in blood supply which can cause irreversible damage. Hardening of the arteries (arteriosclerosis), high blood pressure, thrombosis, stroke and heart attack can all result in hearing loss which is usually permanent. As is well known, cardiovascular health can be due to an unhealthy lifestyle and hearing can be affected by a poor diet, smoking and lack of physical exercise. |
Infectious diseases | There are many infectious diseases, bacterial and viral, which can cause sensorineural hearing loss with some of them typically affecting one ear only. Although not a full list, the more common ones are measles, mumps, meningitis, chicken pox, shingles and influenza. |
Medications | Some medications are known to cause sensorineural hearing loss and these are called ototoxic drugs. Nowadays, these are only used for life-threatening conditions such as certain cancers or serious infections.
Even aspirin can cause hearing loss if taken in regular, larger doses but usually the hearing loss is reversible once the medication is stopped. |
Diabetes | Diabetes should be much better known as a cause of sensorineural hearing loss, especially considering the worrying increase in Type 2 diabetes in the adult population. All diabetics should have regular hearing tests. |
Menieres disorder (syndrome) | Meniere’s disorder (syndrome) is the most common condition involving both hearing loss and balance problems, often with tinnitus in one or both ears. The cause of Meniere’s disorder isn’t known for certain and may involve a number of possible causes.
Sudden attacks of dizziness are a particularly unpleasant aspect of this condition which are often accompanied by a fluctuating hearing loss and low-pitched tinnitus. Even when the dizzy spells stop happening, a permanent hearing loss with persistent tinnitus usually results, sometimes with one ear being much worse than the other. |
Genetic | Hereditary or genetic hearing loss does not always means a person is born with it. Genetic hearing loss can have a late onset such as in Ushers Syndrome which involves progressive loss of both vision and hearing.
Genetic influence can be very difficult to establish as a cause of hearing loss but it’s thought that this is a factor for some people as to when age-related hearing loss begins to occur and may even mean some people are more susceptible to hearing loss from noise exposure. |
Ageing | Age-related hearing loss isn’t just due to deterioration in the cochlea of the inner ear as explained above.
Ageing can also mean that the auditory nerve and hearing centres in the brain can lose the ability to process sound efficiently causing particular problems with more complex sounds such as speech or music. |
Tumour | Although very unusual, a tumour can develop between the inner ear and the brainstem. It’s a benign rather than malignant tumour called an acoustic neuroma or vestibulocochlear schwannoma. It normally grows very slowly, gradually compressing the auditory nerve and may also affect the nearby vestibular (balance) nerve so that there is both hearing loss and balance problems often with tinnitus.
Almost always, the tumour is only on one side, so anyone found to have sensorineural hearing loss and/or tinnitus just in one ear should see their GP for referral to an ENT Consultant for specialist assessment. Bilateral tumours are even rarer and are usually associated with a hereditary condition called neurofibromatosis type 2 (NF2). |
Dementia | Although the subject of much ongoing research, it is already clear that there is an association between untreated/unassisted hearing loss and cognitive decline and dementia. It is not yet fully understood how unassisted hearing loss can accelerate the onset of cognitive decline and dementia. However, it is increasingly clear that hearing loss should never be ignored because the consequences of not seeking professional help for hearing loss may result in greater problems that the hearing loss itself and put a person at significant risk of additional mental health problems. |
Video on the causes of hearing loss
Thanks to Hear-it
Webpage updated: April 2024